What is Dermatomyositis?
The typical characteristic of dermatomyositis is a skin rash (caused by skin inflammation) that precedes or accompanies progressive muscle weakness caused by muscle inflammation and there may also be lung issues. Dermatomyositis may be associated with collagen-vascular or autoimmune diseases, such as lupus.
Dermatomyositis can affect any age group, but is more likely to occur in middle-aged adults. In children, it usually appears between the ages of 5 and 15. It is twice as common in women.
The condition doesn’t generally run in families but there may be genetic factors that could make some people more likely to develop autoimmune conditions such as DM.
The cause of Dermatomyositis is unknown. It may be related to an autoimmune reaction, or may be triggered by a virus or cancer.

Signs and Symptoms
Not everyone has all of the following signs and symptoms as they tend to vary from person to person:
- Red or purplish rash (see right / below)
- Gradual muscle weakness – upper arms, shoulders, neck, hips and thighs on both sides of the body. Occasionally, adults may experience a more rapid onset, however, this may be come common in children with Juvenile Dermatomyositis. As the disease progresses, the muscles begin to waste away (atrophy) and permanently shorten (contracture).
- Joint pain and swelling
- Difficulty swallowing which may cause weight loss and malnutrition.
- Nailfold abnormalities – reddened skin around the fingernails or changes in the blood vessels around the fingernails
- Mechanic’s hands – a roughening and cracking of the skin of the tips and sides of the fingers
- Scalp changes –that resemble psoriasis (scaly, itchy, dry skin patches)
- Interstitial lung disease – some patients with Dermatomyositis develop interstitial lung disease which can cause scarring on the lungs making it harder to breathe
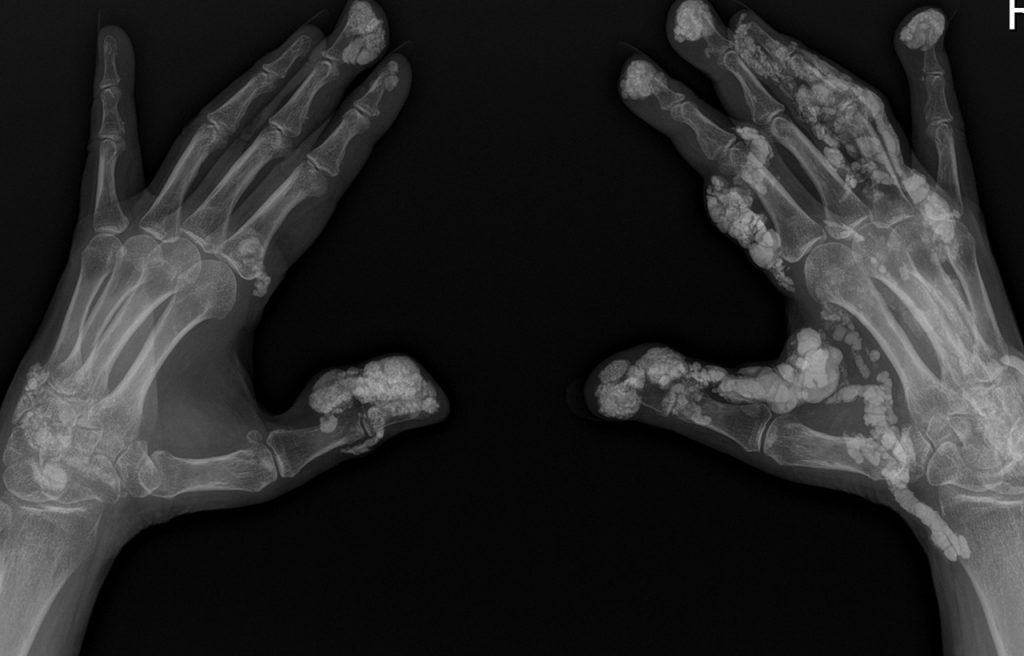
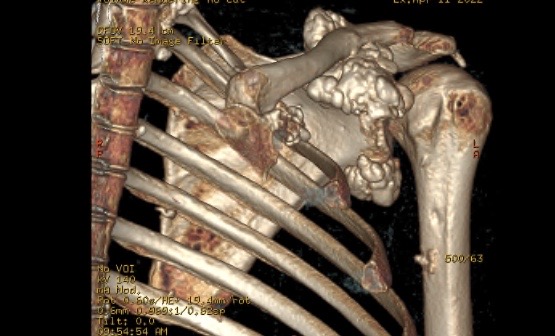
- Calcinosis – painful deposits of calcium salts forming nodules under the skin or in muscles and tendons
- Fever
- Fatigue

Skin Rashes
A red or purplish rash and other skin changes are often the predominant symptom of DM. Sometimes the rash develops before muscle problems occur. Several types of rash may occur:
- Gottron’s papules – red or violet, slightly raised bumps over the knuckles and joints of the top part of the hand that are often scaly
- Gottron’s sign –red or violet coloured patches on the area of skin outside the elbow, knee, or ankle joints
- Shawl sign – a widespread, flat, reddened area that appears on the upper back, shoulders, and back of the neck
- V sign – looks similar to the shawl sign, but appears on the front of the chest in the area of skin exposed by a V-necked t-shirt
- Heliotrope rash –blue/purple rash and swelling on the upper eyelids
- Holster sign – reddish brown skin pigmentation around the buttocks and outer thighs
- Facial erythema – abnormal red skin on the face.
The rashes are made worse by exposure to ultraviolet light (sunlight) and the skin may be scaly, dry and rough.
Some people with Dermatomyositis develop a rash without muscle weakness. This is called Dermatomyositis sine myositis. Others may also have Raynaud’s phenomenon, in which the small arteries in the fingers and toes constrict, causing the skin to look pale or bluish, usually after exposure to cold.
Muscle Weakness
Muscle weakness starts with the muscles closest to the trunk of the body such as those in the hips, thighs, back, upper arms, neck and shoulders. The weakness usually develops over several weeks to months. This causes problems with climbing stairs, getting up out of chairs and lifting objects over the head.
As the condition progresses some people may notice that muscles such as those in the forearms and ankles and wrists become weaker and there may be difficulty in holding the head up.
Muscle pain, tenderness and fatigue can be a significant problem for people with DM. In severe cases breathing problems and trouble chewing, swallowing and speaking can develop.
Other signs and complications
Calcinosis. A very rare complication where deposits of calcium salts can occur underneath the skin or in muscles and tendons. They form hard, painful nodules – known as calcinosis. It occurs in both adult and juvenile forms of DM however, it is more common in juvenile DM. Calcinosis can be very painful if on pressure points or around the face or joints. They can also cause functional disability, contractures and skin ulcers. Various treatments may assist or surgery to remove the deposits may be needed. Sun protection is important.
Approximately 1 in 10 people with Dermatomyositis develop interstitial lung disease which can cause scarring on the lungs making it harder to breather.
Dermatomyositis can cause heart muscle inflammation. People living with DM may also experience an irregular heartbeat (arrhythmia). They also have an increased risk of having a heart attack.
People with inflammatory myopathies, especially adults with Dermatomyositis have an increased risk of cancer. This risk increases with age and involves the same common cancers that affect the general population, including cancer of the lung, breast, prostate, and ovaries. As a result, people with DM may need more frequent cancer screening, especially in the first five years after diagnosis.
DM often occurs in isolation but sometimes it is associated with “connective tissue disorders” such as rheumatoid arthritis, systemic lupus erythematosus (SLE), Raynaud’s disease, scleroderma or Sjögren’s syndrome.
People living with DM may develop aspiration pneumonia caused by breathing food or liquids into the lungs.
In rare cases, inflammation of the fat lying just under the skin, called panniculitis, can also occur, causing tender lumps to form under the skin.
In some cases, inflammation of the blood vessels in other organs such as eyes can occur.
Rare example of severe Calcinosis – calcium deposits in hands, feet and shoulder area.
Anti-MDA5 Dermatomyositis Subtype
Anti-Melanoma Differentiation-Associated gene 5 (MDA-5) Dermatomyositis (MDA5, DM) has been recently identified by researchers as a DM subtype. MDA-5 is a protein used in our immune system to detect the genetic information of viruses. People with Anti-MDA5 DM have autoantibodies that specifically target and attack MDA-5.
Anti-MDA5 DM can be life threatening because it is typically associated with rapidly progressive interstitial lung disease (RP-ILD) Rapidly progressive ILD is reported in over 40% of cases and according to research, is the most important factor predicting survival. It is critical for health professionals to recognise the characteristic skin ulcers and papules associated with Anti-MDA5 DM as early intervention may help to reduce mortality rates.
Some of the signs, symptoms and complications of Anti-MDA5 DM include:
- Higher risk for interstitial lung disease (ILD) including rapidly progressive interstitial lung disease (RP-ILD)
- Increased risk of pneumomediastinum – air in the space between the lungs and around the heart
- Lower incidence of myositis
- Skin ulceration overlying Gottron’s papules , Gottron’s sign , the side of the fingernails and fingertips
- Painful reddish or violet coloured skin patches and firm raised spots, predominantly over the finger creases and palms
- Lower incidence of muscle inflammation
- Prominent nonscarring hair loss
- Mechanic’s hands – a roughening and cracking of the skin of the tips and sides of the fingers
- Eyelid swelling
- Oral ulcers
- Arthritis
- Psoriasis-like rashes (scaly, itchy, dry skin patches)
- Inflammation of the fat lying just under the skin (panniculitis)
- Fever
- Fatigue
Antisynthetase Syndrome
Some people with Dermatomyositis or Polymyositis may also have a further complication, Antisynthetase Syndrome. People with this syndrome have antisynthetase autoantibodies that attack a particular protein essential for our muscles to function well.
There are eight different types of antisynthetase antibodies relevant to Myositis that have been discovered to date. The most common being anti-Jo-1, followed by anti-PL-7 and anti-PL-12. Blood tests can be used to identify the presence of antisynthetase antibodies.
Some of the signs, symptoms and complications of Antisynthetase Syndrome include:
- Muscle inflammation, pain and stiffness
- Interstitial lung disease (ILD)
- Nonerosive arthritis
- Mechanic’s hands – a roughening and cracking of the skin of the tips and sides of the fingers
- Hiker’s feet – a roughening and cracking of the skin of the toes and soles of the feet
- Fever
- Fatigue
- Loss of appetite or unintended weight loss
- Raynaud’s phenomenon – temporary disruption of blood flow to the small blood vessels in extremities. In response to cold or stress, your fingers, toes, tip of the nose, lips and ears can turn blue, feel cold and numb. After the blood flow returns, you may feel tingling and throbbing in the affected areas.
MSAs and clinical features associated with them
from The Myositis Association (USA):
| Autoantibodies | Clinical features |
|---|---|
| Anti-ARS (antisynthetase) | AS syndrome with moderate-to-serve muscle weakness with high muscle enzyme levels, RP, mechanic’s hands, fever, arthritis, and ILD |
| Anti-Jo-1 | Chronic continuous disease course, with clinical symptoms for >two years after diagnosis; mean five-year survival rate = 65%, usually due to ILD; AS syndrome features |
| Anti-PL-7 | AS syndrome with higher frequency of ILD |
| Anti-PL-12 | AS syndrome with higher frequency of ILD |
| Anti-EJ | Dermatomyositis and ILD |
| Anti-OJ | Myositis and ILD |
| Anti-KS | ILD with less myositis |
| Anti-Ha | NA |
| Anti-Zo | Myositis and ILD |
| Anti-SRP | Acute onset NM with severe weakness, high CK, cardiac involvement; refractory to treatment |
| Anti-Mi-2 | Adult DM and JDM with hallmark cutaneous disease, milder myositis with good response to treatment |
| Anti-TIF1-y (anti-p155/140) | CAM in adult DM; severe cutaneous disease in adult DM and JDM |
| Anti-SAE | Adult DM; may present with CADM first |
| Anti-MDA5 (anti-CADM140) | CADM; rapidly progressive ILD |
| Anti-NXP-2 | Predominantly JDM with subcutaneous edema, calcinosis, and servere muscle disease with contractures; increased risk of cancer in some adult DM studies |
| Anti-HMGCR | NM; associated with statin use in adults; severe proximal muscle weakness; partially responsive to immunosuppressive medications; better response to IVIg |
| Anti-cN-1A (Mup44, NT5c1A) | IBM; higher mortality risk |
ARS=aminoacyl-tRNA synthetase; AS syndrome=antisynthetase syndrome; RP=Raynaud’s phenomenon; ILD=interstital lung disease; SRP=signal recognition particle; T1F1-y=transcriptional intermediary factory 1-gamma; NXP-2=nuclear matrix protein-2; SAE=small-ubiquitin-like modifier activating enzyme; MDA5=melanoma-differentiation associated gene 5; CAM=cancer-associated myositis; CADM-clinically amyopathic DM; NA-not applicable/no data.
What causes Dermatomyositis?
The cause of DM is not well understood. It is known that it is an autoimmune condition, in which the body’s immune system mistakenly attacks small blood vessels in the muscles and under the skin. Inflammatory cells surround the blood vessels which eventually leads to degeneration of muscle fibers. What causes this autoimmune reaction is still up for debate. It is thought that in some cases viruses or certain drugs might be a trigger.
Although DM is not considered a genetic disease, there may be some genetic factors that make it more or less likely that the condition will develop.
How is Dermatomyositis diagnosed?
Some of the tests for diagnosing Dermatomyositis include:
- Medical history and physical exam: The diagnostic process is started by a careful look at your medical history and a thorough physical exam. You might be asked whether you have had any difficulty swallowing food and drinks. Your doctor may ask about your ability to carry out common daily activities like climbing the stairs, getting up from a chair or carrying heavy objects such as groceries.
- Blood tests: These are usually the next step. Nearly all people with DM will have high levels of creatine kinase (CK) in their blood. This is a protein that normally resides in muscle but leaks out into the blood when the muscles are damaged. A Myositis Panel blood test may also be done because it may
show up antibodies that indicate a particular form of Dermatomyositis or other autoimmune conditions. Antibodies are proteins made by the immune system. However, some people with DM will have no sign of autoimmune antibodies.
- Muscle biopsy: A muscle biopsy is often needed to give an accurate, definitive diagnosis. It involves removing a small piece of muscle through an incision in the skin. The specimen is examined under a microscope for evidence of blood vessels in the muscles being attacked by immune cells. Muscle cells also appear smaller than normal around the edges of bundles of muscle fibres, and capillaries are scarce in these regions.
DM can easily be confused with many other muscle conditions and is difficult to diagnose, especially in the absence of antibody markers. Other tests that may be done to give extra clues and rule out other conditions include:
- Magnetic resonance imaging (MRI): which can detect changes suggesting muscle inflammation
- Electromyogram (EMG): which can demonstrate abnormal electrical activity in muscles and help distinguish weakness due to muscle disease from weakness due to nerve problems
- Nerve conduction velocity test: measures how fast a nerve impulse travels and how strong it is
- Skin biopsy: Not usually required for DM diagnosis but can be used to rule out other conditions such as eczema or psoriasis.
How is it treated?
DM is a highly treatable disease with some people recovering completely, while others are able to keep the symptoms under control for long periods of time. Treatment involves drugs to control the inflammation that is causing the muscle weakness. No one treatment works for everyone and often a trial and error approach is needed to find the best combination of treatments.
Initial treatment involves high-dose corticosteroids such as prednisolone. Although this is usually effective very quickly, taking these drugs at a high dose for a long period of time carries a high risk of serious side effects. For this reason, the dosage is then tapered to reach an appropriate maintenance dose. However, corticosteroids should never be suddenly stopped or the dose reduced without checking with your doctor first.
Other drugs to suppress the immune system are often given to help reduce the dose of corticosteroid needed. These include:
- Methotrexate
- Azathioprine
- Cyclosporine
- Mycophenolate mofetil
Other drugs that may help some people include cyclophosphamide and tacrolimus. Although most people tolerate these medications, some may experience side effects so it is important to be aware of the potential risks and benefits of each drug and work with your doctor to find the ideal treatment for you.
IVIg therapy is usually considered in severe cases that do not respond to other treatments but is being used more frequently to treat DM. This is an infusion of immunoglobulins (antibodies) extracted from a large pool of donated blood. It is thought that these extra antibodies confuse and interfere with the body’s immune system. More information on IVIg is available here.
If none of the treatments mentioned above are effective, the doctor will first reconfirm the diagnosis of DM. Then drugs that have been approved to treat other autoimmune conditions may be tried such as rituximab or alemtuzumab (for more information on these types of drugs please see ‘What research is being done’ below).
Taking steroids can increase the risk of osteoporosis (brittle bones) so it is important to consider supplements of calcium and vitamin D, and hormone replacement therapy (HRT) in post-menopausal women. In some cases a group of drugs called bisphosphonates may be prescribed to help prevent steroid-induced osteoporosis.
Avoidance of sun exposure during peak hours and use of sunscreen and protective clothing are recommended to avoid worsening the skin aspects of the disease.
Physiotherapy is recommended to keep the joints supple and physiotherapists can supervise an appropriate exercise program. A gentle exercise program, such as hydrotherapy in a swimming pool, can help to maintain strength and wellbeing. Some people may need a cane, walker or even a wheelchair during acute flare-ups of DM and an occupational therapist and/or physiotherapist can help with arranging these.
Careful attention to a healthy diet can help with the management of the symptoms, especially when taking corticosteroids as they can lead to significant weight gain which may cause extra strain on the muscles.
Regular monitoring of creatine kinase (CK) levels, muscle strength, breathing, swallowing and heart function is recommended to allow any problems to be anticipated and treated.
What research is being done?
Much of the research into DM focuses on understanding precisely why and how the immune system attacks the blood vessels, which will lead to better treatments for the disease.
Monoclonal Antibodies
Several new drugs developed for other autoimmune diseases or for treating people who have had an organ transplant are now being tested for myositis. Some anti-cancer drugs that target cells of the immune system also show promise for inflammatory myopathies. Most of these drugs are so-called “monoclonal antibodies” and have the abbreviation “mab” at the end of their name.
Antibodies are proteins produced by the immune system that target a protein or type of cell in the body and as a result it is destroyed. An antibody preparation that is produced in the laboratory containing identical antibodies is called “monoclonal”. When used as drugs, monoclonal antibodies are designed to target a part of the body that is harmful, for example cancer cells or a component of the immune system that has become overactive in an autoimmune disease.
Lenabasum
Lenabasum is a drug that binds to an activates CB2 receptors in our body. These receptors may be involved regulating immune system responses such as inflammation.
Despite positive results from earlier studies, Lenabasum failed to meet both the primary and secondary endpoints in a recent randomised, double-blind, placebo-controlled, Phase 3 trial on DM patients.
KZR- 616
Immunoproteasome are a group of proteins expressed in immune cells that regulate cell function by digesting and breaking down damaged or unneeded proteins. KZR- 616 is an immunoproteasome inhibitor design to “reduce inflammation by targeting dysfunctional immune cells involved in autoimmunity – , such as T -cells and B -cells – , without causing widespread immunosuppression in patients.”
A phase 2 randomised, double-blind, placebo-controlled, crossover multicentre study to evaluate the safety and efficacy of KZR-616 in treating DM and PM is currently underway. The estimated study completion date is April 2022.
BAF312 (Siponimod)
Another drug recently tested in clinical trials for myositis is BAF312 (Siponimod). This drug, which was developed by Novartis Pharmaceuticals, is designed to act on the cells of the immune system to inhibit their migration to the location of the inflammation. It was hoped that this, in turn, would lead to reduced inflammation and muscle damage. Unfortunately, siponimod has not been found to be effective in treating DM in two research trials.
Tocilizumab
Tocilizumab is one example of a monoclonal antibody. This drug was developed for rheumatoid arthritis and targets a protein called “interleukin 6 receptor” which plays an important role in immune responses and inflammation. Unfortunately, in a recent phase 2 multicentre, randomised, placebo-controlled trial of tocilizumab on 36 patients with DM/PM, the trial failed to meet its primary and secondary endpoints.
Rituximab
Another monoclonal antibody is rituximab which was developed to treat blood cancers such as leukemia and works by destroying one type of white blood cell (B cells). Rituximab has also been shown to be effective for a range of autoimmune disorders.
The Rituximab in Myositis (RIM) trial completed in 2010, was the largest trial of the rituximab in people with inflammatory myositis. It was a double blinded, randomized placebo phased clinical trial that included 195 patients (75 PM, 72 DM, and 48 juvenile dermatomyositis (JDM)). The research findings suggest that rituximab may be effective for people with these types of Myositis. Since this trial, other smaller studies have also demonstrated that rituximab may be effective for PM and DM.
Apremilast
Apremilast is a drug that inhibits an enzyme in inflammatory cells called phosphodiesterase 4 (PDE4). It is thought that PDE4 may cause overactive inflammation inside the body.
A phase 2, open label, single arm, single centre clinical trial of apremilast in DM patients was recently completed in April 2021. However, the results of this trial are not yet available.
Abatacept
Abatacept is a modified antibody designed to reduce inflammation by interfering with and reducing the activity of immune cells in our body, called T-cells. It is currently used as an effective treatment for many people living with arthritis. A phase 3, randomized, double-blind clinical trial to evaluate the efficacy and safety of abatacept in adults with PM, DM, Autoimmune Necrotizing Myopathies, OM and JM is currently underway. The estimated study completion date is October 2024.
Other research
A list of clinical trials for DM can be found on the clinicaltrials.gov website. Note that some of these studies are “observational” which means that no new drug or treatment is given.
Stay up to date
Research is moving forward at a fast pace, so this research summary may not be up-to-date at the time of reading. One of the best ways to stay up to date with the latest on research is to become a member. We regularly provide updates on research in our bi-monthly member newsletters.